Abstract
Background:
Graft-versus-host disease (GVHD) is a dreaded complication after allogeneic hematopoietic stem cell transplantation (allo-HSCT). Such inflammatory diseases are fostered by damage to the intestinal barrier after transplantation. Consequently, the integrity and regeneration of the intestinal barrier is a key factor in the prevention of GVHD. On one side the main driver for regeneration of damaged gut epithelium are intestinal stem cells (ISC), but on the other side these cells are themselves primary targets of donor-derived T cells. One known mechanism of T cell mediated damage to the stem cell compartment is through IFN-γ dependent ISC toxicity. Yet, little is known about how T cells are contributing to the regeneration of damaged tissue after allo-HSCT and GVHD.
Methods:
To address this, we used preclinical models for allo-HSCT and GVHD including transplantation of recipient mice with escalating doses of Wildtype or IFN-γ-deficient allogeneic T cells and in the presence or absence of the JAK-1/2 inhibitor ruxolitinib. Intestinal regeneration was assessed by RNA-seq, flow cytometry and a newly established ex vivo organoid recovery assay. GVHD outcome was assessed by clinical scoring, histology and survival. Additionally, we established an allogeneic co-culture system of murine or human intestinal organoids with CD4+ conventional T cells or T regs -/+ Ruxolitinib. Effects on organoid growth and cell death were assessed by size measurements and manual counting after passaging.
Results:
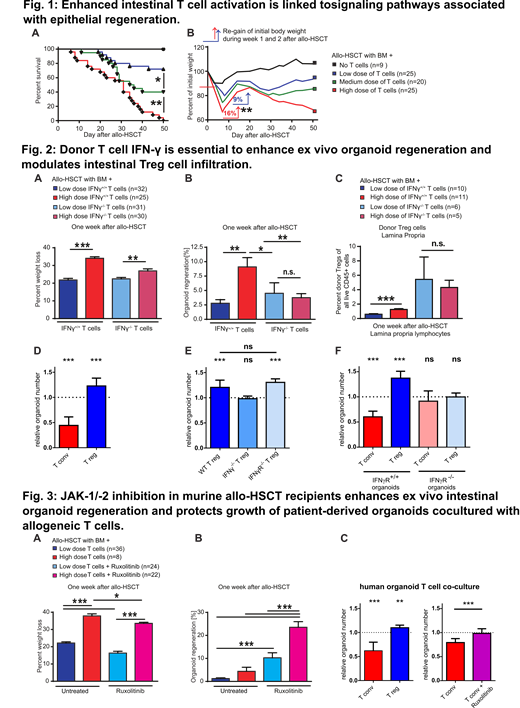
We here demonstrate that recipient mice with increasingly dense intestinal infiltration by allogeneic T cells not only developed more severe GVHD (Fig. 1A), but also showed augmented recovery potential early after allo-HSCT (Fig. 1B). This was associated with intestinal gene signatures related to epithelial regeneration and protection from GVHD. Utilizing ex vivo cultures of intestinal organoids generated from murine allo-HSCT recipients, we found that development of GVHD but also regenerative capacity of ISCs were dependent on interferon (IFN)-γ-producing T cells in the intestine (Fig. 2A-B). Mice with fulminant GVHD and enhanced organoid recovery showed accumulation of intestinal regulatory T cells (Tregs) (Fig. 2C). Ex vivo, T regs nurtured growth of intestinal organoids in an IFN-γ dependent manner (Fig. 2D-E). This effect was diminished in intestinal organoids lacking IFNγR signaling, but was independent of T reg intrinsic IFNγR signaling (Fig. 2E-F). Intriguingly, treatment of murine allo-HSCT recipients with the JAK-1/2 inhibitor ruxolitinib enhanced epithelial organoid regeneration and numbers of intestinal Tregs (Fig. 3A-B). Similarily, growth of human intestinal organoids co-cultured with allogeneic T cells could be augmented by ruxolitinib treatment (Fig. 3C). We thus propose that the level and differentiation of infiltrating intestinal T cells determines both ISC damage and epithelial regeneration during immune-mediated tissue injury, leading to a sensitive equilibrium that can be modulated by therapeutic intervention. We also provide evidence that ruxolitinib improves ISC regeneration via IFNγ-producing Treg cells.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal